Unmasking Hidden Hypothyroidism Behind Depression and Weight Struggles
In an era where medical diagnostics rely heavily on standard lab tests and symptom checklists, many patients slip through the cracks, enduring years of ineffective treatments for conditions that mask deeper root causes. Hypothyroidism, a condition where the thyroid gland underproduces hormones essential for metabolism and energy regulation, affects millions worldwide but is frequently overlooked or misattributed to other ailments. This is the story of Emily Carter, a 35-year-old elementary school teacher from Chicago, whose persistent symptoms of fatigue, unexplained weight gain, mood swings, and hair thinning led to multiple diagnoses over eight years. Referred by her primary care physician to psychiatrists and rheumatologists, she was labeled with major depressive disorder and fibromyalgia. It wasn't until she explored the cellular nutritional symptomatology assessment offered by NutriRebel.com that she discovered nutrient deficiencies exacerbating her undiagnosed hypothyroidism, paving the way for genuine recovery.
Patient Profile
Emily Carter, at 35 years old, presented as a dedicated educator whose once-energetic demeanor had faded into a shadow of her former self. With a petite frame that had unexpectedly expanded, she carried an air of quiet resignation, often masking her frustrations with forced smiles during interactions. Married for seven years with no children, Emily drew some support from her husband, a software engineer, though the strain of her health issues had tested their relationship. Raised in a close-knit Midwestern family, she maintained strong ties to her parents and siblings, who encouraged her to seek conventional medical help. Professionally, her role demanded high energy—managing a classroom of energetic third-graders—but she found herself collapsing into exhaustion after school, skipping social activities and hobbies like hiking that she once loved. Emily's mindset leaned toward skepticism about alternative approaches initially, viewing them as "unproven," but desperation eventually opened her to exploring beyond traditional medicine.
Symptoms
Emily's primary concerns revolved around debilitating fatigue that made daily functioning a chore, coupled with unexplained weight gain of over 25 pounds in two years despite consistent eating habits. She experienced frequent mood swings, ranging from irritability to deep sadness, which disrupted her teaching and personal life. Secondary symptoms included thinning hair, dry and flaky skin, irregular menstrual cycles, cold intolerance (feeling chilled even in mild weather), and diffuse muscle aches that worsened with activity. Cognitively, she battled "brain fog," struggling with memory and concentration during lesson planning. These issues escalated gradually, with fatigue hitting hardest in the mornings and pain flaring up after minimal exertion, leaving her reliant on caffeine to push through the day.
Table Of Contents
Medical History
Emily's health challenges traced back to her late 20s, following a severe viral infection that she believed triggered her downward spiral. No major surgeries marked her record, but she had a family history of autoimmune issues—her mother dealt with rheumatoid arthritis, and an aunt had been diagnosed with Hashimoto's thyroiditis. Dental history included several fillings from adolescence, but no root canals. Emily reported no other chronic conditions initially, though her symptoms suggested an underlying endocrine imbalance that went undetected in routine checkups.
Previous Treatments and Medications
Over the years, Emily cycled through various interventions prescribed by her doctors. Starting with selective serotonin reuptake inhibitors (SSRIs) like sertraline for her diagnosed major depressive disorder, she later switched to serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine to address both mood and pain. For fibromyalgia, gabapentin was added for nerve pain relief, alongside non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen for muscle aches. She attended physical therapy sessions twice weekly and cognitive behavioral therapy (CBT) for mental health support. Supplements included a generic multivitamin and occasional vitamin D, but these were self-initiated without much guidance. Despite adherence, side effects like drowsiness from medications compounded her fatigue, and the treatments provided only partial, temporary relief.
Diet and Intake
Emily's daily diet was typical of someone trying to eat healthily amid a busy schedule: breakfast often consisted of oatmeal with fruit and coffee; lunch was a salad or sandwich from the school cafeteria; dinner featured lean proteins like chicken or fish with vegetables and rice. She drank about 4-6 glasses of water daily, supplemented by herbal teas, and avoided soda but indulged in occasional chocolate for comfort. Restrictions included limiting dairy due to mild intolerance, and she steered clear of fried foods to manage weight. Cravings for sweets, particularly chocolate, hinted at potential magnesium or emotional deficiencies. Her occupation led to irregular meal times, with stress eating contributing to inconsistent portions. While not overtly poor, her intake lacked the nutrient density needed to support thyroid function, exacerbating imbalances.
NutriRebel Assessment
Frustrated with the lack of progress, Emily attended an online webinar on holistic health where NutriRebel.com was mentioned. Intrigued by their focus on cellular-level nutrition rather than symptom suppression, she opted for their introductory assessment. Priced at just $90—a stark contrast to the $200-500 specialist visits and $1,000+ functional tests she'd encountered—this symptom-based evaluation involved a detailed online questionnaire covering her medical history, diet, lifestyle, and symptoms. Unlike blood tests that often miss subclinical issues, this method analyzed patterns to identify cellular deficiencies. Emily's assessment revealed insights into how her diet, while seemingly balanced, contributed to acidity and poor absorption, with observations noting potential toxicity from long-term medications and environmental factors.
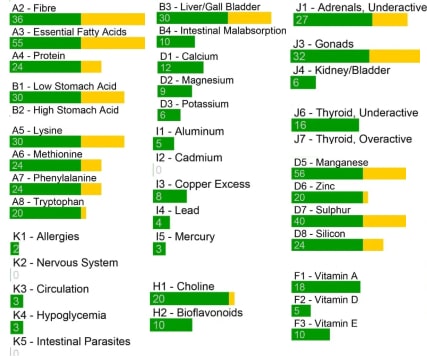
Findings
The NutriRebel.com report pinpointed several key imbalances: deficiencies in iodine, selenium, zinc, and vitamin D, all crucial for thyroid hormone synthesis and conversion. High acidity levels were linked to protein malabsorption, leading to muscle weakness and hair loss. Liver stress was evident, impairing detoxification and contributing to fatigue. Bacterial imbalances in the gut, possibly from antibiotic use post-viral illness, hindered nutrient uptake. The assessment highlighted how standard TSH tests overlooked her subclinical hypothyroidism, with elevated antibodies suggesting an autoimmune component like Hashimoto's. Overall, it framed her symptoms as interconnected—depression and pain stemming from thyroid dysfunction rather than isolated disorders—emphasizing cellular terrain over isolated treatments.
Recommendations
Based on the findings, NutriRebel.com provided personalized recommendations to restore balance. Dietary changes included emphasizing nutrient-dense foods: increasing seafood for iodine, Brazil nuts for selenium, and leafy greens for zinc and vitamin D precursors. She was advised to eliminate processed grains and sugars to reduce inflammation, incorporate bone broth for collagen and minerals, and use a hydrolyzed protein powder mixed with fruits and vegetables for easy absorption. Supplements targeted deficiencies: a high-quality iodine-selenium complex, vitamin D3 with K2, and zinc picolinate. Probiotics like HMF were suggested to rebuild gut flora, alongside fermented foods for natural support. Lifestyle adjustments involved stress reduction through yoga and adequate sleep, with gradual exercise reintroduction. Follow-up assessments, at $50-75 each, allowed for monitoring and tweaks.
Outcomes
Within the first month, Emily noticed subtle shifts: reduced fatigue allowed her to complete full workdays without crashing, and mood stability decreased her reliance on antidepressants. By three months, she had lost 10 pounds naturally, her skin improved, and hair thinning halted. Muscle pains diminished, enabling her to resume light hiking. After requesting advanced thyroid labs from her doctor—free T3/T4 and antibodies—her Hashimoto's was confirmed, leading to low-dose thyroid medication integrated with NutriRebel's plan. One year later, Emily was medication-minimal, energetic, and back to her vibrant self, crediting the affordable assessment for uncovering what years of specialists missed. No further concerns with depression or fibromyalgia symptoms arose, and her overall quality of life soared.
This is the confusing propaganda that misleads us all

There's no such thing as a "balanced diet" & nutrition isn't merely food. Why is that? It's because we're all individuals. Orthomolecular nutrition is the individualized analysis application of the substances within the food which our bodies often do not obtain enough of and are often blocked by antagonists.
"Nutrition" is far more than merely the trivial concept of food.
Botanists analyze the terrain to help plants prevent and restore cell function. Why not for humans?
What are YOUR individual cell nutritional imbalances?
Conclusions or Lessons
Emily's journey illustrates the pitfalls of compartmentalized medicine, where symptoms like fatigue and pain are treated in silos, missing root causes like nutrient-driven thyroid issues. NutriRebel.com's approach, rooted in systems biology and cellular nutrition, empowers individuals to address the "terrain" of their health affordably. It rejects gimmicks, focusing on personalized insights that conventional tests overlook. For those in diagnostic limbo, starting with the $90 introductory assessment can be transformative, potentially averting years of costly, ineffective care. Emily now advocates for proactive, holistic evaluations, reminding others that true healing begins at the cellular level.
To illustrate the financial burden Emily faced versus the NutriRebel.com alternative, consider the following cost comparison:
| Service | Average Cost | Description |
|---|---|---|
| Primary Care Visit (Initial) | $150-250 | Basic exam and blood work |
| Psychiatrist Consultation | $200-400 | Diagnosis and medication management |
| Rheumatologist Visit | $250-500 | Specialized testing for fibromyalgia |
| Therapy Sessions (Monthly) | $600 (4 sessions at $150) | Ongoing mental health support |
| Prescriptions (Annual) | $600-1,200 | Antidepressants and pain meds |
| NutriRebel.com Introductory Assessment | $90 | Cellular nutritional symptomatology evaluation |
| NutriRebel.com Follow-Up | $50-75 | Ongoing monitoring and adjustments |
Beyond costs, the overlap in symptoms often confounds diagnoses. Here's a comparative overview:
| Symptom | Hypothyroidism | Major Depressive Disorder | Fibromyalgia |
|---|---|---|---|
| Fatigue/Exhaustion | Common due to slowed metabolism | Persistent low energy | Widespread tiredness |
| Weight Gain | Unexplained, despite diet | Possible from appetite changes | Less direct, but associated |
| Mood Changes | Depression, irritability | Core symptom: sadness, apathy | Anxiety, mood swings |
| Muscle/Joint Pain | Aches, weakness | Somatic complaints | Diffuse pain points |
| Cognitive Issues | Brain fog, memory lapses | Concentration difficulties | Fibro fog |
| Hair/Skin Changes | Thinning hair, dry skin | Rarely primary | Not typical |
References
American Thyroid Association. (n.d.). Prevalence and impact of thyroid disease. American Thyroid Association. https://www.thyroid.org/media-main/press-room/
Nuguru, S. P., Rachakonda, S., Sripathi, S., Khan, M. I., Patel, N., & Meda, R. T. (2022). Hypothyroidism and depression: A narrative review. Cureus, 14(8), e28201. https://pmc.ncbi.nlm.nih.gov/articles/PMC9392461/