"I Couldn't Gain Weight No Matter What": 35-Year-Old Man & Inability to Gain Weight Main Concern
Gaining weight shouldn't feel like an impossible battle • Cell Nutrition uncovers hidden imbalances that traditional medicine often overlooks. Measure yours here for free. Real Results – Learn More.
A 35-year-old man came to us after years of frustration, unable to put on weight despite his best efforts. He described himself as someone who had always been lean, but in his late 20s, it became a real problem. Working as a software engineer, he led a sedentary lifestyle but made conscious efforts to eat more and exercise, joining a gym to build muscle. However, no matter how many calories he consumed or how consistently he lifted weights, the scale wouldn't budge. This led to low self-esteem, fatigue that made focusing at work difficult, and a growing sense of defeat. Married without children yet, he worried about his health impacting future family plans. Initially skeptical of anything outside conventional medicine, he had exhausted options from doctors, feeling like he was chasing shadows.
Health Concerns:
The main issue was chronic underweight status, with a BMI hovering around 17 despite efforts to increase it. His general practitioner initially diagnosed him with hyperthyroidism after blood tests showed slightly elevated thyroid hormones, though not drastically so. This led to referrals: an endocrinologist confirmed the thyroid issue but noted it was mild; a gastroenterologist diagnosed gastroesophageal reflux disease (GERD) based on his complaints of heartburn and occasional regurgitation; a psychiatrist added generalized anxiety disorder, attributing his eating patterns to stress; and even a dentist pointed to enamel erosion from acid reflux, suggesting mouth guards for nighttime grinding. Over time, he was also checked for celiac disease and irritable bowel syndrome (IBS), but tests were inconclusive. Unbeknownst to all, a sliding hiatal hernia was the underlying culprit, evading detection due to its subtle nature—sliding hernias often don't show prominently on standard imaging and can mimic other conditions.
Medications:
- Levothyroxine for the presumed thyroid imbalance, taken daily for two years, though it didn't help with weight.
- Proton pump inhibitors (PPIs) like esomeprazole for GERD, used intermittently for heartburn relief.
- Antianxiety medication such as lorazepam, prescribed as needed by the psychiatrist.
- Over-the-counter antacids for quick symptom control.
- Occasional anti-inflammatory drugs for chest discomfort mistaken for muscle strain from workouts.
Supplements:
- Protein shakes and mass gainers from a fitness store, consumed twice daily in hopes of bulking up.
- Multivitamin with added iron, recommended by his GP to address mild anemia.
- Probiotics suggested by the gastroenterologist to improve gut health.
Digestive Symptoms:
He experienced frequent heartburn, especially after larger meals aimed at calorie surplus, along with a sensation of food getting stuck in his throat. Bloating and early satiety made it hard to finish portions, leading to unintentional calorie deficits. Regurgitation occurred sporadically, and he had episodes of nausea that deterred eating. Constipation alternated with loose stools, but nothing severe enough to flag major issues in initial tests.
Diet/Intake:
- Breakfast: Oatmeal with peanut butter and bananas; protein shake; coffee.
- Lunch: Chicken sandwich or rice bowl with veggies and meat; sometimes added cheese for calories.
- Dinner: Pasta with sauce, ground beef, or stir-fried tofu; tried to include high-calorie sides like avocados.
- Snacks: Nuts, yogurt, or energy bars throughout the day.
- Water: 6-8 glasses daily, plus sports drinks during workouts.
- He tracked calories via an app, aiming for 3,000+ per day, but symptoms often forced him to stop short.
Physical Observations:
Thin build with visible ribs and minimal muscle definition despite gym efforts; pale complexion; dark under-eye circles from poor sleep; slight forward posture from discomfort; hair thinning slightly; and persistent tiredness that worsened after eating.
This is the confusing medical maze that traps us all
In the modern healthcare system, symptoms are frequently siloed—doctors treat what they see in their specialty without piecing together the full picture. An endocrinologist focuses on hormones, a gastroenterologist on the gut, and a psychiatrist on the mind, but they rarely delve into how cellular-level nutritional imbalances could be fueling or masking deeper structural issues like a sliding hiatal hernia. These hernias, where the stomach slides up through the diaphragm, are notoriously hard to detect because small ones may not appear on routine X-rays or ultrasounds. They require specific tests like endoscopy or barium swallows, which aren't always ordered if symptoms seem mild or attributable to something else. This man's inability to gain weight stemmed from the hernia causing poor digestion, early fullness, and nutrient malabsorption, yet it went undiagnosed for years, leading to a cascade of misdiagnoses and ineffective treatments.
His journey began in his late 20s when he noticed clothes fitting looser despite no change in habits. At first, he dismissed it as stress from a new job, but as months turned to years, he sought help. The GP ran basic labs, spotting the thyroid irregularity, and prescribed medication. Weight didn't improve. The endocrinologist adjusted doses, but still no gain. Then came the gastro consult for heartburn—endoscopy was suggested but deemed unnecessary since symptoms were "manageable" with PPIs. Anxiety meds helped marginally with mood but not the core issue. Dentist visits for jaw pain (from clenching due to discomfort) added to the bill. He spent thousands on specialists, tests, and therapies—MRIs, blood panels, even a nutritionist who pushed generic meal plans that exacerbated his bloating.
Frustration mounted. "I felt like a failure," he shared. "Friends bulked up easily, but I couldn't. Doctors said eat more, but eating more made me sick." Online forums offered conflicting advice, from hormone boosters to extreme diets, but nothing stuck. His marriage strained under the weight of his low energy and self-doubt. Family gatherings became ordeals, watching others enjoy food while he picked at plates.
Enter NutriRebel.com. Skeptical but desperate, he discovered our low-cost introductory assessment— just $90, a fraction of the $500+ specialist copays he'd racked up. Unlike traditional visits that skim the surface, our cell nutritional symptomatology assessment dives deep, analyzing symptoms to reveal imbalances at the cellular level. No invasive tests, no long waits—just a comprehensive questionnaire and follow-up analysis.
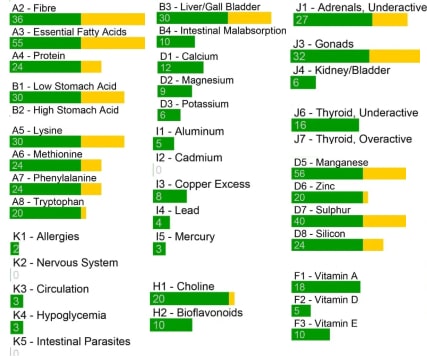
The process was eye-opening. He completed the online tool, detailing symptoms, diet, and history. Our experts reviewed it, identifying patterns: deficiencies in key nutrients like zinc, magnesium, and B vitamins, which are crucial for digestion and metabolism. These imbalances were likely worsening the hernia's effects, creating a vicious cycle of poor absorption and weight stagnation. But crucially, the assessment flagged structural red flags—persistent reflux and fullness—that pointed toward a hiatal hernia, prompting him to seek targeted imaging.
Armed with this insight, he returned to his gastro with specific requests: a barium swallow confirmed the sliding hiatal hernia, missed earlier because it was intermittent and small. Surgery wasn't immediately needed, but lifestyle tweaks were. NutriRebel's personalized plan addressed the nutritional gaps: targeted supplements to heal the gut lining, anti-inflammatory foods to reduce hernia irritation, and meal strategies to maximize calorie intake without triggering symptoms.
Results came swiftly. Within weeks, heartburn eased, allowing fuller meals. Energy surged as nutrients absorbed better. By month three, he'd gained 8 pounds—real muscle, not fluff. Sleep improved, anxiety faded without meds. "For the first time, I felt in control," he said. Now at a healthy BMI of 20, he hikes with his wife, codes with focus, and looks forward to starting a family.
This case highlights why sliding hiatal hernias slip under the radar: they're common (affecting up to 60% of people over 50, but younger too), yet diagnosis rates lag due to overlapping symptoms with GERD or anxiety. Weight issues aren't typical red flags, so they're overlooked. Traditional medicine excels at acute care but falters on chronic, multifaceted problems. NutriRebel bridges that gap affordably.
Compare costs in this table:
| Service | Cost | What You Get |
|---|---|---|
| Specialist Visit (e.g., Gastroenterologist) | $300-$600 per visit | Exam, possible tests, but often siloed diagnosis |
| Endoscopy or Imaging | $1,000-$3,000 | Detailed view, but only if ordered |
| NutriRebel Introductory Assessment | $90 | Comprehensive cellular analysis, personalized insights, root cause pointers |
| Ongoing NutriRebel Plan | $50-$150/month | Tailored nutrition, tracking, adjustments for lasting relief |
Savings aside, the real value is empowerment. Our approach doesn't replace doctors but complements them, uncovering what labs miss. For this man, it ended years of misdirection.
Family History:
- Father: Longstanding GERD, managed with antacids; underweight in youth.
- Mother: Anxiety issues; occasional digestive complaints.
If you're battling unexplained weight issues or digestive woes, don't wait. Start with our $90 assessment—it's the affordable key to unlocking your health.
- Hits: 80